Can a Psychologist Refer to a Psychiatrist — and What It Means for Your Mental Health
/https://freudly.ai/media/pages/images/dae14902-3052-4920-ad13-8fc15fea485a.png)
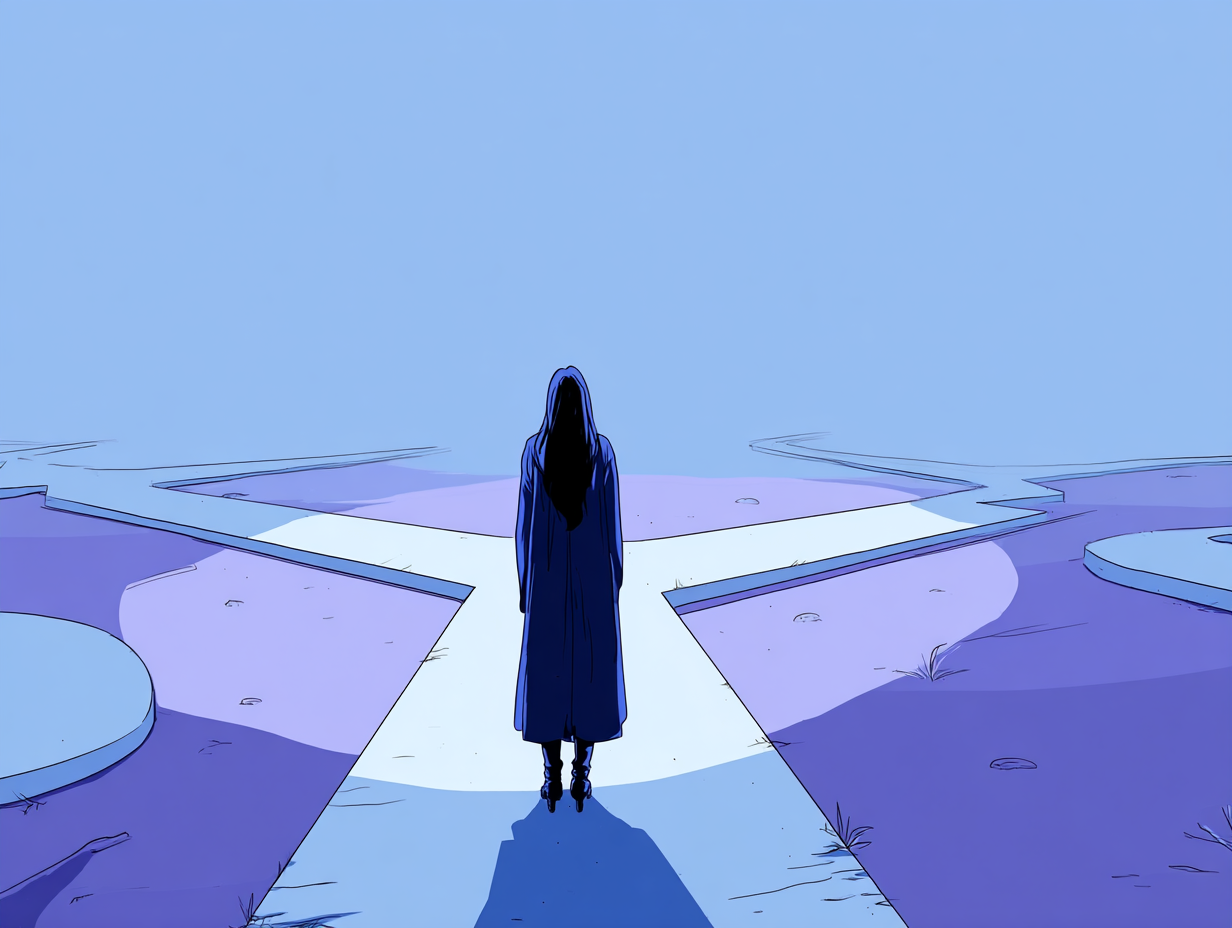
Feeling confused about the difference between a psychologist and a psychiatrist is common. Many people start therapy hoping to find relief through conversation and emotional insight - then feel uncertain when their psychologist mentions a possible referral. The question often arises: can a psychologist refer a psychiatrist, and what does that actually mean for me?
In the U.S., a psychologist can refer a psychiatrist when they believe medication, a medical evaluation, or combined care could help you recover more effectively. This referral doesn’t mean therapy has failed or that something is “wrong” with you. It means your clinician recognizes that your symptoms may benefit from medical input alongside continued therapy.
In this guide, you’ll learn how psychologists and psychiatrists work together, when a referral happens, what to expect during the process, and how to maintain trust in your care team. You’ll also discover practical coping tools for the waiting period and clear signs that it’s time to seek professional help.

What Happens When a Psychologist Refers a Psychiatrist - Understanding the Roles of Each Professional
When a psychologist refers a psychiatrist, it often signals a positive shift toward more complete care - not a failure of therapy. In U.S. mental health practice, psychologists and psychiatrists frequently work side by side, offering complementary skills that together create a fuller picture of recovery. Understanding each role can ease uncertainty and help you feel more informed when your clinician suggests a referral.
At its core, a psychologist focuses on how you think, feel, and behave - using evidence-based therapies to help you change patterns, build insight, and improve coping. A psychiatrist, on the other hand, is a medical doctor who evaluates how the brain and body interact, prescribes medications when necessary, and monitors physical health factors that influence mood and behavior.
Education and Licensing: How Psychologists and Psychiatrists Differ
Psychologists typically hold a Ph.D. or Psy.D., complete thousands of supervised clinical hours, and specialize in psychotherapy and behavioral assessment. They are licensed by state psychology boards.
Psychiatrists hold a medical degree (M.D. or D.O.) and complete residency training in psychiatry, allowing them to prescribe medication, perform physical exams, and order lab tests. They are licensed as physicians.
Important to know: while both are mental-health professionals, the difference lies in approach - psychologists address cognitive and emotional patterns through talk therapy, whereas psychiatrists focus on the biological and pharmacological side of treatment.
Collaboration in U.S. Mental Health Care
In integrated care settings, it’s common for a psychologist to refer a psychiatrist for a joint treatment plan. The psychologist continues therapy sessions, while the psychiatrist evaluates whether medication might support emotional stability or symptom relief.
According to the American Psychological Association (APA) and SAMHSA, this type of collaboration - sometimes called co-treatment - improves outcomes for people experiencing depression, anxiety, trauma, or complex mood disorders. It allows each professional to focus on their expertise while sharing information (with your consent) to coordinate care safely.
Why a Psychologist May Suggest a Psychiatric Consultation
- therapy progress has plateaued and symptoms remain severe;
- physiological signs (like insomnia, appetite loss, or psychomotor slowing) suggest biological involvement;
- risk factors such as suicidal thoughts or psychosis appear;
- medication could reduce distress enough for therapy to be more effective.
It’s not a sign that your psychologist can’t help you. Instead, it reflects ethical practice - recognizing when additional medical insight may enhance your progress.
Psychologist vs. Psychiatrist Roles
| Role | Psychologist | Psychiatrist |
|---|---|---|
| Education | Ph.D. / Psy.D. | M.D. / D.O. |
| Focus | Behavior, cognition, emotions | Brain chemistry, medical treatment |
| Methods | Talk therapy, CBT, ACT, DBT | Medication, physical evaluation |
| Can prescribe meds? | Only in limited U.S. states | Yes (nationwide) |
| Works with | Psychiatrists, counselors, families | Psychologists, primary-care physicians |
| Typical session | 45–60-minute therapy | 20–30-minute medication management |
Understanding the Balance
When a psychologist refers a psychiatrist, you don’t have to choose one over the other. Many Americans see both concurrently - therapy addresses behavior and thought patterns, while medication manages biological symptoms. Research from Harvard Health and the National Institute of Mental Health shows that combining both can significantly improve long-term outcomes for moderate to severe conditions.
On the flip side, if your symptoms are mild and you’re responding well to therapy, your psychologist may simply mention psychiatric consultation as an option - not a requirement. The key takeaway: a referral is about expanding your support network, not replacing it.
Why a Psychologist Refers a Psychiatrist - When Therapy Alone May Not Be Enough
When a psychologist refers a psychiatrist, it usually means your therapist has noticed signs that a biological or medical factor may be affecting your symptoms. This doesn’t mean therapy has failed. In fact, psychologists refer psychiatrists precisely to strengthen treatment - ensuring that every possible angle, from thought patterns to brain chemistry, is addressed.
Let’s take a closer look at why this referral can be a turning point, not a setback.
Clinical Reasons for Referral
Therapy and medication often work best together when symptoms are severe, persistent, or interfere with daily life. According to the American Psychological Association (APA) and National Institute of Mental Health (NIMH), psychologists refer psychiatrists when certain patterns emerge:
- Therapy plateaus: When progress slows despite consistent sessions.
- Biological symptoms appear: Persistent sleep issues, appetite changes, or physical agitation may signal neurochemical imbalance.
- Safety concerns: Thoughts of self-harm, hallucinations, or extreme mood swings require medical evaluation.
- Diagnostic clarification: A psychiatrist can assess whether a mood, psychotic, or neurodevelopmental disorder may be present.
Ethical Responsibility Under APA Guidelines
Here’s the thing: psychologists in the U.S. are ethically required to act when a client’s needs fall outside their professional scope. The APA’s Ethical Principles of Psychologists and Code of Conduct state that clinicians must ensure clients receive appropriate treatment, even if that means referring out for additional care.
That’s why psychologists refer psychiatrists when they suspect medication could help - it’s not about stepping back, but stepping up for the client’s well-being. Referrals show professional integrity and respect for evidence-based care.
DSM-5-TR Context: When Combined Treatment Is Recommended
The DSM-5-TR, used by U.S. clinicians for classification, recognizes that certain disorders - such as major depressive disorder, bipolar disorder, and panic disorder - often respond best to a combination of psychotherapy and pharmacotherapy. In these cases, psychologists refer psychiatrists to coordinate the medical aspects while maintaining therapeutic work on behavioral and emotional change.
According to the Mayo Clinic and Harvard Health Publishing, integrated treatment improves remission rates and prevents relapse. Medication can stabilize mood or anxiety levels, allowing therapy to go deeper once the most distressing symptoms subside.
Common Referral Scenarios
| Condition or Symptom | Why Referral Helps | Typical Combined Plan |
|---|---|---|
| Major depression | Medication can lift energy and motivation | SSRI + CBT sessions |
| Panic disorder | Reduces physiological panic symptoms | CBT + short-term benzodiazepine or SSRI |
| Bipolar disorder | Stabilizes extreme mood fluctuations | Mood stabilizer + psychotherapy |
| OCD | Supports therapy-based exposure work | SSRI + ERP (Exposure and Response Prevention) |
| Suicidal thoughts | Urgent medication and crisis plan | Psychiatrist + psychologist co-treatment |
Why Therapy Alone Isn’t Always Enough
Sometimes, emotional progress is blocked by factors beyond conscious control - genetic predispositions, hormonal changes, or medication side effects from other health conditions. In these moments, a psychologist’s referral to a psychiatrist creates balance between insight-driven and biological care.
Many clients notice that once medication helps regulate mood or reduce panic intensity, therapy becomes more effective. The ability to focus, reflect, and apply coping tools increases dramatically when the nervous system isn’t in constant distress.
A Reassuring Perspective
When your psychologist refers a psychiatrist, it’s not a signal of weakness or “failure to improve.” It’s a professional recognition that healing sometimes requires more than one expert. Collaboration ensures your care remains ethical, comprehensive, and tailored to you - the hallmark of modern U.S. mental-health practice.
How Psychologist–Psychiatrist Referrals Work in the U.S. Health System
When a psychologist refers a psychiatrist, the next step is often more logistical than emotional. Understanding how the U.S. healthcare system manages mental health referrals can make the process less intimidating and more transparent. Whether you’re using private insurance, public coverage, or paying out of pocket, knowing how psychologist–psychiatrist referrals work helps you stay in control of your care.
The Referral Process Step-by-Step
- Clinical discussion. Your psychologist explains why a psychiatric evaluation may help and invites your input. You have full autonomy to accept or decline - therapy continues regardless.
- Consent and release. If you agree, your psychologist may ask for written consent to share relevant notes with a psychiatrist. This allows coordinated care under HIPAA privacy laws.
- Finding the right psychiatrist. The psychologist often provides referrals from a trusted professional network or your insurance list. Some practices have in-house psychiatrists or partner clinics.
- Scheduling and evaluation. The psychiatrist conducts a comprehensive medical and mental health assessment, possibly including lab tests or screening tools. They may recommend medication, lifestyle adjustments, or further testing.
- Feedback loop. With your permission, both clinicians communicate periodically to align therapy goals with medication management. This teamwork ensures consistent progress and minimizes overlap or gaps in care.
Insurance and Out-of-Network Referrals
Here’s the thing - insurance can affect how quickly you see a psychiatrist, but a referral from your psychologist often simplifies the process.
- Private insurance: Many U.S. plans don’t require a referral to see a psychiatrist, but having one helps justify medical necessity for reimbursement.
- Public plans (Medicare/Medicaid): A documented referral can increase coverage approval for psychiatric services.
- Out-of-network care: If your preferred psychiatrist isn’t covered, your psychologist’s referral letter may still help secure partial reimbursement or flexible spending approval.
- Telepsychiatry: Since 2020, most major insurers have expanded telehealth coverage, making virtual psychiatric consultations accessible nationwide.
If cost is a concern, your psychologist may recommend community mental-health centers, teaching hospitals, or sliding-scale clinics supported by SAMHSA.
Confidentiality and HIPAA Compliance
The collaboration between psychologists and psychiatrists follows strict U.S. federal and state privacy laws. According to HIPAA, no information can be exchanged without your signed consent.
- Psychologists can share therapy notes only with your explicit authorization.
- Psychiatrists may send medication updates or treatment summaries if you consent.
- You can revoke information-sharing at any time.
- Crisis exceptions exist only if there’s imminent danger to self or others - in which case, safety takes priority.
Transparency is key. Your psychologist should explain exactly what information would be shared and why. Most clients find that open collaboration actually builds trust, as both professionals align on consistent goals rather than working in isolation.
The Bigger Picture: Integrated Care in the U.S.
The Substance Abuse and Mental Health Services Administration (SAMHSA) and American Psychiatric Association (APA) endorse collaborative or “integrated care” models - where psychologists, psychiatrists, and primary-care doctors communicate regularly. This approach leads to better outcomes, fewer medication errors, and greater satisfaction for clients.
When your psychologist refers a psychiatrist, it’s part of this larger movement toward holistic, patient-centered care - where mind and body are treated together, not separately.
What to Expect After a Psychologist Refers a Psychiatrist - Therapy, Medication, and Follow-Up
When a psychologist refers a psychiatrist, many people wonder what happens next. Will therapy stop? Will everything now focus on medication? In reality, most clients continue seeing both professionals - one focusing on emotional understanding and behavioral change, the other on medical stabilization. The process is collaborative, flexible, and centered on you.
Here’s a simple breakdown of what to expect once the referral is made.
The First Psychiatric Appointment
The psychiatrist begins by learning your full story. They’ll review your psychological background, medical history, current symptoms, and lifestyle factors. The goal is to understand how your body and mind interact. During this first meeting, you can expect:
- a detailed discussion of your mood, energy, sleep, and thought patterns;
- possible screening questionnaires or lab work to rule out medical issues;
- questions about family mental-health history;
- time to share any concerns or fears about medication.
Psychiatrists emphasize informed consent - meaning they’ll explain potential medication benefits, side effects, and timelines before prescribing anything. You always have the right to decline or request alternatives.
Will You Still See Your Psychologist?
Absolutely. When a psychologist refers a psychiatrist, the psychologist remains your primary therapeutic partner. You’ll continue regular sessions to explore emotions, relationships, and stress patterns. Therapy may even become more effective as medication helps stabilize mood or reduce anxiety intensity.
In most collaborative settings:
- the psychologist handles emotional processing, coping skills, and behavioral strategies;
- the psychiatrist monitors medication response and adjusts dosages;
- both professionals (with your consent) coordinate through brief updates or shared reports.
Important to know: Psychiatrists typically do not replace therapy; they complement it. Most evidence-based treatment plans integrate both psychological and medical care for best results.
Coordinating Medication and Therapy Effectively
To make psychologist–psychiatrist collaboration seamless, communication and boundaries are essential. Here’s how clients can keep both forms of care aligned:
- Be open about changes. Let your psychologist know if medication is helping, causing fatigue, or shifting emotions. This helps tailor therapy goals.
- Track side effects. Keep a journal of physical or mood changes. Share this with your psychiatrist and psychologist to adjust treatment safely.
- Attend follow-ups. Medication typically requires check-ins every few weeks at first. Regular sessions prevent dosage issues or withdrawal symptoms.
- Ask for coordination. Give both professionals permission to share updates if you’re comfortable. Many clients sign a limited-release form to streamline collaboration.
- Stay patient. It can take several weeks for medication to reach full effectiveness. Your psychologist will help you manage expectations and emotional reactions during this adjustment phase.

Emotional Adjustments During Combined Care
Starting medication can bring mixed feelings - relief, hope, but also uncertainty. You may worry about dependency or personality change. These thoughts are normal. Discuss them openly in therapy. Many people find that addressing these fears early reduces stigma and helps maintain trust in the treatment process.
When a psychologist refers a psychiatrist, the shared goal is recovery, not control. Medication doesn’t erase emotions; it simply reduces intensity so you can process experiences more effectively in therapy.
Long-Term Follow-Up and Maintenance
Over time, your treatment plan evolves based on progress and comfort level. Some people see psychiatrists for a few months, others for years - especially when managing chronic conditions. Common next steps include:
- gradually tapering off medication under medical supervision;
- revisiting therapy frequency as stability increases;
- continuing periodic psychiatrist check-ins;
- reassessing goals every 3–6 months to ensure balance and satisfaction.
Healing is rarely linear. Some phases may feel slower than others, but collaboration between both professionals keeps recovery steady and safe.
How to Talk with Your Psychologist About a Psychiatrist Referral
When a psychologist refers a psychiatrist, emotions can range from relief to discomfort. Some clients feel grateful that their therapist is taking extra steps to support them; others fear being “handed off.” In reality, referrals are part of ethical and collaborative mental health care - and talking about them openly can deepen trust between you and your therapist.
Here’s how to navigate that conversation with confidence and clarity.
Expressing Concerns Without Shame
Many people hesitate to bring up fears about medication, stigma, or control. Remember that your psychologist’s goal is partnership, not persuasion. They want to hear your thoughts. Try to share feelings openly:
- “I trust your judgment, but I’m nervous about seeing a psychiatrist.”
- “Can you explain what made you think a psychiatric evaluation might help?”
- “Will we still meet regularly if I start medication?”
Therapists appreciate honesty. It helps them clarify intent and provide reassurance that referral doesn’t mean therapy is ending - it means care is expanding.
Questions to Ask Before the Referral
Before scheduling your first psychiatry appointment, you can ask your psychologist a few practical questions:
- “Do you have psychiatrists you’ve collaborated with before?”
- “How will communication between you and the psychiatrist work?”
- “What kind of medication might they consider - and how would that fit with my therapy goals?”
- “Can I choose whether you two share information or keep records separate?”
- “What should I do if I don’t feel comfortable with the psychiatrist you recommend?”
These questions aren’t confrontational - they’re empowering. The more informed you are, the smoother the process becomes.
Maintaining Trust in the Therapeutic Relationship
When your psychologist refers a psychiatrist, trust may feel momentarily shaken. It’s natural to wonder if your therapist believes you’re “too difficult” to treat. The truth is the opposite: a psychologist who refers you shows professional responsibility and care.
Here’s how to maintain connection and trust during the transition:
- Keep communicating. Share updates about your psychiatric visits. Discuss how medication affects your emotions and thoughts in therapy.
- Be transparent about doubts. If you feel uneasy about medication or side effects, bring that into session. Your psychologist can help you process it safely.
- Reaffirm shared goals. Remind yourself that both professionals work toward the same outcome - your stability, well-being, and autonomy.
- Set boundaries. If you prefer limited communication between providers, discuss exactly what can be shared.
- Acknowledge progress. Notice and celebrate small improvements, whether emotional insight or symptom relief. This reinforces a sense of teamwork.
Here’s the thing: Good therapy doesn’t end with a referral; it evolves. Psychologists and psychiatrists often collaborate for months or even years, helping clients address both emotional and physiological needs. When communication is open, the process becomes empowering rather than intimidating
Reframing the Conversation
Ultimately, talking about a referral is an opportunity to practice what therapy teaches - honesty, curiosity, and self-compassion. If a psychologist refers a psychiatrist, it reflects care, not rejection. It shows your therapist is invested in your long-term health and ready to share the load with another expert.
Being able to discuss this step directly strengthens the therapeutic alliance - and reminds you that recovery is a shared journey, not a solitary one.
Self-Help While Waiting for a Psychiatrist Appointment - What You Can Do Now
When a psychologist refers a psychiatrist, it may take weeks before you can schedule your first visit. The waiting period can feel uncertain - symptoms may still fluctuate, and you might worry about getting worse. The good news is that there are effective, research-backed strategies you can use right now to support yourself while waiting for that first psychiatric consultation.
Here’s how to stay grounded and maintain emotional balance in the meantime.
Grounding and Mindfulness Techniques
Simple grounding and mindfulness practices help keep your nervous system from entering constant “fight-or-flight” mode. These skills complement therapy and reduce anxiety until medical treatment begins.
Try a few of these:
- 5–4–3–2–1 sensory grounding: Name five things you can see, four you can touch, three you can hear, two you can smell, and one you can taste.
- Diaphragmatic breathing: Inhale slowly for four counts, exhale for six, repeat for two minutes.
- Progressive muscle relaxation: Tense and release muscle groups from head to toe to lower physical tension.
- Mindful walking: Pay attention to your breath, steps, and surroundings - even five minutes outside can calm racing thoughts.
These techniques help interrupt spirals of worry and give your body a signal that you’re safe.
Journaling and Symptom Tracking
Therapists and psychiatrists alike value self-observation. Journaling helps capture emotional patterns and provides useful information for your psychiatrist’s assessment.
While waiting for your appointment:
- record mood changes, sleep patterns, and energy levels daily;
- note specific triggers or events that worsen or improve symptoms;
- write down any questions or concerns you’d like to ask your psychiatrist;
- track any side effects from over-the-counter supplements or existing medications.
Bringing this journal to your first appointment gives the psychiatrist a more accurate baseline and helps shorten the evaluation process.
Healthy Routines to Stabilize Mood
Small daily habits can strengthen emotional regulation and improve resilience. Even modest consistency matters.
- Stick to a sleep schedule. Go to bed and wake up around the same time each day.
- Eat balanced meals. Avoid skipping food or relying on caffeine and sugar spikes.
- Move your body. Walk, stretch, or do light exercise - movement helps regulate cortisol and serotonin levels.
- Limit substance use. Alcohol, recreational drugs, and excess caffeine can amplify anxiety and disrupt sleep.
- Stay socially connected. Talk to trusted friends, family, or peer support groups instead of isolating.
When to Seek Urgent Care or Call 988
If symptoms suddenly worsen or you begin to experience hopelessness, thoughts of self-harm, or intense agitation, waiting is no longer appropriate - you need immediate help.
In the United States:
- call or text 988 to reach the Suicide and Crisis Lifeline for free, 24/7 confidential support;
- if you or someone else is in immediate danger, dial 911 or go to the nearest emergency department;
- you can also contact local crisis stabilization centers or walk-in clinics for same-day evaluation.
Your psychologist can guide you through this process or help you create a crisis safety plan during sessions.
Using Therapy to Prepare
While waiting to see the psychiatrist, use therapy sessions to:
- explore any fears about medication or psychiatric evaluation;
- set realistic expectations for what you want from medication;
- discuss healthy coping tools and relapse prevention;
- practice communicating openly about physical and emotional symptoms.
When your psychologist refers a psychiatrist, therapy becomes a safe space to stay engaged, grounded, and informed - helping you step into the new phase of care with confidence.
Psychologist Refers Psychiatrist as a Team Approach - A Path Toward Recovery and Balance
When a psychologist refers a psychiatrist, it marks a turning point toward more balanced, integrated care. Instead of seeing the referral as an endpoint, think of it as an expansion - two experts joining forces to help you heal more effectively. The psychologist brings deep understanding of your emotions and patterns; the psychiatrist contributes medical insight into the brain’s chemistry and how physical health interacts with mood. Together, they form a safety net that holds you steady as you recover.

The Value of Team-Based Mental Health Care
Integrated care means you’re not navigating the system alone. When your psychologist refers a psychiatrist, both professionals collaborate to design a plan that fits your life and unique biology. You benefit from multiple perspectives, fewer blind spots, and more consistent monitoring. According to the American Psychiatric Association (APA) and SAMHSA, this model significantly reduces relapse rates for conditions such as major depression, anxiety, and bipolar disorder.
- coordinated treatment goals so therapy and medication reinforce each other;
- fewer misunderstandings about progress or side effects;
- better crisis prevention through shared communication;
- improved motivation, since both providers track your milestones.
Breaking the Stigma Around Psychiatric Referrals
For decades, stigma has kept many people from accepting psychiatric help. Words like “referral” or “medication” can sound intimidating, even threatening. Yet when a psychologist refers a psychiatrist, it’s no different from a family doctor sending you to a cardiologist - it’s simply connecting you to a specialist.
Let’s be clear about what it doesn’t mean:
- It doesn’t mean you’re “too broken” for therapy.
- It doesn’t mean your psychologist can’t handle your case.
- It doesn’t mean you’ll automatically be prescribed strong medication.
What it does mean is that your clinician values comprehensive care. They see your well-being as multifaceted - emotional, biological, social - and want to ensure every part of you gets the support it needs.
The Emotional Arc of Recovery
At first, the process might feel overwhelming. You might have to meet new professionals, manage appointments, or adjust to medication side effects. It’s okay to feel uncertain. Healing isn’t linear - it bends, stalls, and restarts. Your psychologist and psychiatrist expect this, and they build flexibility into your plan.
Over time, as symptoms stabilize, therapy sessions often shift from crisis management to growth - strengthening boundaries, relationships, and meaning. Many clients describe this stage as finally “getting their life back.” Medication helps regulate the storm; therapy helps you navigate the ocean once it calms.
The Long-Term Payoff of Collaboration
When your psychologist refers a psychiatrist, you gain more than medical input - you gain an entire framework for sustainable recovery. Integrated care improves consistency, accountability, and self-awareness. Over months or years, this partnership may evolve: perhaps you taper off medication, reduce therapy frequency, or transition to maintenance check-ins.
The ultimate goal isn’t dependence on professionals but empowerment. When two experts work together, they model healthy communication and boundaries - skills you can internalize in your own life. You learn to coordinate, advocate, and care for yourself the same way your providers care for you.
Finding Balance and Moving Forward
If your psychologist has referred you to a psychiatrist, try to view it as an act of care. It means they see your potential for progress and want to expand the resources available to you. Accepting help from both professionals isn’t a sign of weakness - it’s an investment in strength, balance, and long-term stability.
Recovery is a process of learning to live, not just to survive. When your psychologist and psychiatrist collaborate, you don’t have to choose between emotional insight and biological understanding - you receive both, integrated into one compassionate plan.
References
1. American Psychological Association. Understanding Psychologists, Psychiatrists, and Other Mental Health Professionals. 2023.
2. National Institute of Mental Health. Mental Health Medications. 2023.
3. Mayo Clinic. Psychiatrist vs. Psychologist: What’s the Difference? 2023.
4. Substance Abuse and Mental Health Services Administration (SAMHSA). Integrated Care Models in Behavioral Health. 2022.
5. Harvard Health Publishing. Medication, Therapy, or Both? 2022.
6. American Psychiatric Association. Collaborative Care and Integrated Behavioral Health. 2023.
Conclusion
When a psychologist refers a psychiatrist, it reflects professionalism, not failure. It means your therapist recognizes that mental health involves both emotional and biological factors - and wants to give you the most effective support available. Working with both specialists allows you to stabilize symptoms, deepen insight, and build lasting resilience.
If you’ve recently received a referral, try to view it as a partnership rather than a handoff. You’re still the central member of your care team, and both professionals are there to help you reach stability, balance, and well-being. Healing takes time, but collaboration speeds the process and reduces relapse risk.
If you’re in crisis or feeling unsafe, call or text 988 to reach the Suicide and Crisis Lifeline in the United States. If there’s immediate danger, call 911 or go to the nearest emergency department.
Frequently Asked Questions
Can a psychologist refer a psychiatrist directly?
Yes. In the United States, a licensed psychologist can refer a psychiatrist directly when medication or medical assessment may help improve treatment outcomes. This is part of ethical and integrated care.
Does a referral mean I’ll have to take medication?
Not necessarily. A referral means the psychiatrist will evaluate whether medication could be beneficial. You decide together based on the results, comfort level, and treatment goals.
Will my psychologist and psychiatrist share information?
Only if you give written consent. Under HIPAA, you control what information is shared between your providers. Collaboration usually improves coordination but is never automatic without your approval.
Do I need a referral to see a psychiatrist in the U.S.?
Most private insurance plans don’t require a psychologist’s referral, but having one may speed approval or reimbursement. Public plans like Medicaid often prefer a documented referral for coverage.
Can I keep seeing my psychologist after starting medication?
Yes. Combined care is standard practice. Psychologists focus on therapy and coping strategies, while psychiatrists manage medication. Together, they create a balanced treatment plan.
What if I can’t afford a psychiatrist?
Ask your psychologist about community clinics, university programs, or telepsychiatry options. Many states offer sliding-scale services supported by SAMHSA for individuals without insurance.